Edited by Brendan Striano, Grace Xiong, and Harry Lightsey - 7/1/2021
Fracture Types
- Compression Fractures
- Burst Fractures
- Flexion Teardrop Fractures
- Extension Teardrop Fractures
Exam Pearls
Ensure patient is in well-fitted C-collar
Full BUE and BLE Neuro exam
- (Strength, Sensation, Reflexes, Hoffman, Babinski, Clonus, Rectal Tone +/- Bulbocavernosus, Tenderness to palpation)
- Good to get RN early because will need help with rolling pt for rectal / spine palpation
Workup
Radiographs: CT Cervical Spine (the majority of these consults will come having been diagnosed on CT)
Other imaging:
- if definitively non-operative, obtain upright (standing if possible, if not, sitting) XR Cervical Spine (AP + Lat) in ED or prior to discharge (for clinic comparison)
- MRI C-Spine (stat); specify if there is neurologic deficit warranting further investigation
- CT Angiogram Neck or MR Angiogram Neck - indicated if there is injury that extends into the Transverse foramen (potential vertebral artery injury) - uncommon in these injury patterns
- if vertebral injury present, most pts asymptomatic, but good to know if pt is dependent on their remaining Vertebral artery in the event pt needs surgery
- Requires either a Vascular Surgery or Neurosurgery consult (depending on where the injury is / locoregional patterns of who “owns” the vertebral artery)
Labs: Pre-op labs (in case injury is operative)
Other:
- Need to identify whether pt takes chronic anticoagulation
- Need to beware patients with long fusion segments
- Surgical Fusion, Ankylosing Spondylitis, Diffuse Idiopathic Skeletal Hyperostosis (DISH)
Management
Need for acute intervention:
- Yes, all subaxial C-spine fx pts should be placed into a c-collar until full work-up complete
- Some Fracture patterns can be definitively managed with C-collar
- Acute neurologic compromise requires urgent surgical intervention
Injury Based Treatment Decision:
Compression Fractures
- Wedge fracture of the vertebral body without involvement of the posterior vertebral body cortex
- By definition, no retropulsion into the canal
- Be wary regarding potential posterior ligamentous complex (PLC) injury i.e. facet fx, facet asymmetry, as this would suggest mechanical instability
- Can pursue MRI to assess PLC if uncertain
- Amenable to non-operative management +/- C-collar if neurologically intact and no suggestion of mechanical instability
Burst Fractures
- Vertebral body fracture with involvement of the posterior vertebral body cortex and at least some degree of retropulsion (even if minimal)
- Assess PLC, i.e. facet fx, facet asymmetry, as these suggest instability
- Can assess PLC w/ MRI as needed
- If neurologically intact and mechanically stable, can treat with C-collar
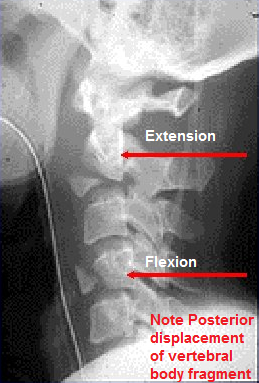
Flexion Teardrop Fracture
classically , the anterior column fails in compression with posterior column failing in tension Often, there is an antero-inferior vertebral body fragment w/ the posterior body translated posteriorly into the canal Neurologic injury is common Mechanical instability is common
**These often present with Spinal Cord Injury and need Stat MRI C-Spine and emergent surgical intervention. Good to alert fellow / attending of these injuries early.
Do not need to have consult “wrapped” up - Need to give fellow/attending lead time”
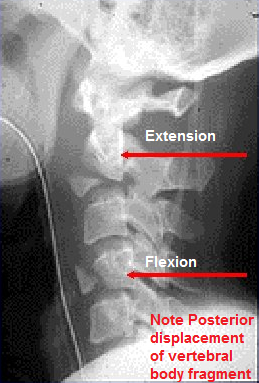
Extension Teardrop Fracture
- An avulsion fragment of the antero-inferior vertebral body by the Anterior Longitudinal Ligament
- Neurologic injury and Mechanical instability are rare
- Must differentiate from a flexion teardrop fracture (as the antero-inferior fx fragment can appear similar)
- If truly Extension Teardrop, treat with C-collar
Weight-bearing and range of motion: if managing definitively with C-collar, it should be maintained at all times
Type of immobilization: C-collar, bed rest is reasonable if pt mechanically unstable injury and pt just came into ED
Admission or discharge status:
- if definitively non-operative, OK to get XR Cervical spine in ED and discharge patient
Many of these injuries will occur in elderly geriatric patients who, even if fracture is safe for discharge, will need PT assessment, possible placement from ED or even admission
- if neurologic compromise, these patients will need to have their care (labs, imaging, etc.) expedited en route to the OR for emergency surgery
Anticoagulation:
- Does not need anticoagulation for this injury alone if isolated injury and non-operative treatment
- if warrants surgical intervention, no anticoagulation
Special circumstances do arise (e.g. - surgical C-spine injury in a pt w/ an active PE), but these are extraordinarily rare and need Fellow/Attending discussion
Antibiotics: None needed
Surgical Indications
Absolute:
- Neurologic Compromise
- Most common in Burst and Flexion Teardrop patterns
- Need to alert fellow / Attending immediately, but most patients get emergent MRI and then OR
- Maintain in C-collar in best in interim
- See Acute Spinal Cord Injury pathway page
Mechanical Instability
- Often these do not need emergent surgery, but do need to be stabilized
- Still want to inform Fellow/Attending overnight as they will need to orchestrate / organize their next AM differently knowing that there is an acute subaxial C-spine that needs stabilization
Relative: None
Not an indication: None