Edited by Phil Grisdela and Matt Fury - 7/1/2021
Initial
Vitals
Assess for hemodynamic instability via heart rate, blood pressure, and mental status
Beware, bradycardia and hypotension as may be sign of neurogenic shock.
Primary Survey
Things that can kill you in minutes - “ABCDE”
A - Airway: is the patient able to phonate / protect their own airway (generally tested via ability to talk)
B - Breathing: Breath sound bilaterally (eval for pneumothorax)
C - Circulation: HR, central and distal pulses (all four extremities, any asymmetry should raise concern for vascular injury)
D - Disability / Deformity
E - Exposure: Remove all clothing to allow for complete secondary
Glasgow Coma Score:
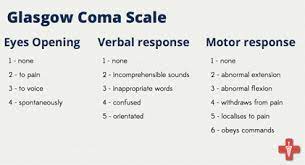
“T” denotes intubation - will commonly be intubated for airway protection at GCS 8
Delta of GCS is useful for prognostication
Secondary Survey - identifying injuries prior to imaging
-Run by ED or Gen Surg team.
-Ortho Team: Identify areas with deformity, crepitus, open wounds over bones or joints. Includes rolling the patient to assess for spine injury, rectal tone
Tertiary Survey:
- Essentially a H&P completed when the patient is alert and oriented without significant distracting injuries to assess for other missed injuries.
- Frequently done on the floor or ICU
Workup
Radiographs:
Traumas should get a CXR at a minimum.
If concern for pelvic injury via mechanism or d/t HD instability, advocate for AP pelvis.
Can't Miss: Pubic widening, SI disruption, Hip Dislocation, Hip Fracture
Other imaging:
Generally speaking, single view extremity XRs slow down care and do not significantly improve care. Rare exceptions such as reducing a dislocated large joint (e.g. native hip) in an otherwise stable patient prior to CT - only to prevent the need for a second CT post-reduction.
Trauma pan scan is CT head and C spine, then chest-abdomen-pelvis.
Labs: CBC, BMP, Coags, Lactate (under 2.5), Type and Screen, PT/INR, tox screen can be helpful
Other: Presentation: “Patient arrived as a (“code trauma”, etc), after (mechanism of injury), on arrival was (tachycardic or not), (normotensive, hypotensive, hypertensive), GCS , Primary survey (intact or not), secondary survey notable for . Imaging notable for (CXR, AP pelvis, any specific ortho injuries, CT pelvis, CT c spine). Injury burden is (orthopaedic and non-orthopaedic). Admitted to . Plan for pending *** clearance from other services.
Management
Need for acute intervention: Good to splint obviously deformed extremities, but do not hold up travel to CT, OR, or ICU just to splint.
Should irrigate and open fractures / traumatic arthrotomies and recommend antibiotics (see below)
Weight-bearing and range of motion: Situationally dependent. Often these evolve quickly and if any concern, keep pt NWB or on bed rest until further information gathering
Type of immobilization: Situationally dependent, but in critical polytraumas, be sure to have splints well-padded to prevent iatrogenic injury (intubated / head injury patients won't communicate that splint is digging in)
Admission or discharge status: Situationally dependent. Ok for Ortho admission if stable with isolated orthopaedic trauma
Anticoagulation: Dependent on injury burden, otherwise typical Ortho trauma DVT prophylaxis is appropriate
Antibiotics: Essentially only for open fractures, in which case, as early as possible (ideally <1h) Cefazolin 2g q8h (Gustillo Anderson I or II) or Ceftriaxone 2g q24h (Gustilla Anderson III)
When in doubt, give antibiotics - better to overcall than under call