Edited by Christina Liu and CJ Nessralla - 7/1/2021
Descriptors
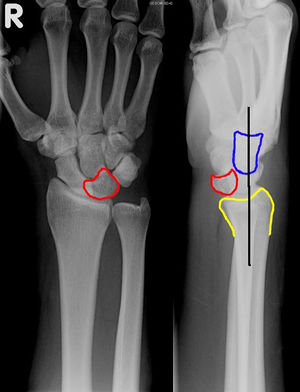
Perilunate and Carpal Dislocations
Exam Pearls
Hand exam
Key: Important to make sure neuro intact as there is a high risk of acute compartment syndrome
Deformity and carpal prominence can sometimes be seen
Workup
Radiographs: PA/lateral/oblique XR of the wrist in neutral position
Other imaging: None
Perilunate dislocation: Lateral XR - capitate no longer sitting in lunate cup
Lunate dislocation: PA XR showing piece of pie sign, Lateral XR showing lunate no longer in line with distal radius and capitate
Labs: optional: preop labs if unable to close reduce in ED/OR.
Other: NA

Management
Hand consults should be staffed with attending/fellow prior to definitive management.
Need for acute intervention: Yes, immobilization with reduction though high risk of failing reduction and needing to reduce and pin in OR. Bedside ED reduction performed with finger traps, elbow at 90, 5-15lbs of traction for 10-15 minutes to relax soft tissues. For dorsal dislocations: extend the wrist, pull traction, flex the wrist.
Weight-bearing and range of motion: NWB, no ROM wrist
Type of immobilization: AO short arm splint
Admission or discharge status: ED Obs for monitoring of acute carpal tunnel syndrome and/or OR if unable to get reduction in ED
Anticoagulation: NA
Antibiotics: NA
Surgical Indications
Absolute: Failed attempt at closed reduction Concern for acute compartment syndrome
Relative:
Timing of surgery
Acute injury
Closed reduction + splint in ED to minimize damage to median nerve/cartilage vs urgent OR reduction if failed ED attempt
Clinic FU: ORIF, ligament repair, CTR
Commonly: decreased grip strength + stiff
Proximal row carpectomy: chronic injury > 8 weeks
Total wrist arthrodesis: chronic injuries with degenerative changes of capitate and/or lunate fossa (fair amount)
Not an indication: NA